Microbiome in human health
We all know that the microbiome is an integral part of a human body, but one will be surprised to know the actual significance of microbiome in overall health, be it physical or psychological. The human microbiome is an unimaginably huge array of microorganisms that live in and on the human body with about 100-fold genetic material as that of human genome. Just to be clear, we have trillions of microorganisms consisting of thousands of different species. So yes, we are not actually who think we are!!!
Some interesting facts
- The microbiome composition and load varies for each person creating a unique network
- Each person’s microbiota weighs approximately 2 kilograms- Yes, you’re actually 2 kilos less heavy!!
- Gut microbiome contains as many as 5,000 different species of bacteria- hard to imagine, isn’t it?
- Our gut is wired with neurons and neurotransmitters (Now we know why we say “gut feeling”) and healthy microbes are key for the proper functioning of gut-brain axis
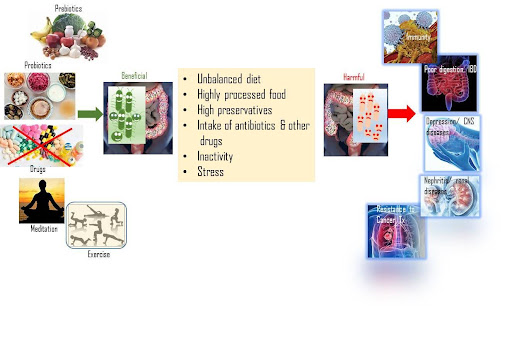
While the microbiome consists of both helpful and harmful microbes, in a healthy body they typically co-exist without any issues. But, when there is a disturbance in that balance (dysbiosis) either due to illness, diet or prolonged use of certain medications such as antibiotics, then we become more prone to diseases. Microbiota are in fact an essential component of human body that stimulate the immune system, metabolize some toxins and synthesize certain vitamins (Vit. B12 and K) and amino acids.
Emerging scientific literature
In recent years, the importance of microbial research is being explored increasingly as one can see from the increase in the number of publications across various therapy areas, including oncology, autoimmune diseases, infectious diseases, CNS diseases, and so on.
In cancer, significance of microbiota, both positive and adverse has clearly been demonstrated. For e.g. Fusobacterium nucleatum, and Clostridium spp. have been shown to be associated with poor prognosis and involved in the progression of colorectal, esophageal, pancreatic, oral, breast and gastric cancers. Similarly, Butyricimonas and Actinomyces, were abundant in cases with recurrent esophageal cancer and Clostridium spp was more abundant in patients with failure of immunetherapy and chemotherapy. On the contrary, E. faecalis and family Ruminococcus have been associated with significantly better clinical outcomes during anti-PD-1 immunotherapy, in hepatocellular carcinoma trials. In another study of advanced cancer patients, treatment with immune checkpoint inhibitor showed a favourable outcome, including increased PFS and OS in the presence of Prevotella copri and Faecalibacterium prausnitzii. More importantly, the microbiota composition in these patients was similar to healthy individuals.
Further, GWAS studies have unveiled critical causal associations, both positive and negative, between different family of bacteria and specific kidney diseases, including nephrotic syndrome, glomerulonephritis, membranous nephropathy and chronic kidney diseases. Understandably, in the progression from inflammation to carcinogenesis in IBD and colitis, interplay between immune cells and gut microbiota plays an important role. Similarly, both positive and negative causal relationships have been demonstrated in diseases that we likely would not have imagined, such as intra-vertebral disc damage (Eubacterium coprostanoligenes), glaucoma (negative effect: Oxalobacteraceae, Eggerthella; positive effect: Bilophila, LachnospiraceaeUCG010) and others. The list goes on and on about any pathological condition that one could think of!!
In CNS related diseases, pre-clinical and clinical trials have demonstrated the role of disbiosys in the onset and progression of depression via regulating the gut-brain axis. In a fecal microbial diversity investigation done in more than 1500 subjects, 3 bacterial species were shown to have a strong associated with depression. Interestingly, these bacteria were involved in the synthesis of GABA, glutamate and butyrate that are key neurotransmitters for depression.
To make the argument even more stronger, there’s one clinical trial that is being conducted in combination with immune checkpoint inhibitor (ICI), where a combination of a live bacterial product BMC128 is being used in phase I clinical trials! BMC128 is a consortium of 4 different bacteria that naturally inhabit the human intestinal tract with specific potential to enhance immune response and facilitate anti-tumor immunity.
Our ancient understanding of gut health
While on one hand, we are beginning to understand the importance of microbiome in human health and the underlying molecular mechanism, in our ancient system of ‘Ayurveda’, gut health was always given prime importance!! According to Ayurveda, all diseases begin in the gut. When our digestive fire burns appropriately, we’re better at digesting what we consume and feel more energetic, clear- minded, and enthusiastic about life. As we saw earlier, latest research suggests that our gut microbiome is extremely important for immunity. From an Ayurveda perspective, it is said that immunity is positively correlated with ‘ojas (life essence)’ that is produced as a by-product of healthy digestion. Ojas is associated with radiant skin, balanced emotions, strong immunity, and overall good health.
The digestive health and microbiome health are intricately linked and if they are efficient in their function, it can lead to the production of what is called as ‘ama’ or digestive toxins. When our digestion is weak, our body struggles to assimilate nutrients and eliminate ‘ama’. Signs of ama in the gut include bloating, indigestion, allergies, etc. and if left unchecked, it can lead to clogging of the numerous communication channels across the body leading to all kinds of health issues, including mental, emotional challenges and weakened immunity.
So, overall, it is obvious that food plays a major role in gut health apart from genetics and environment. Accordingly, consumption of balanced food with probiotic (with beneficial microbiome) and prebiotic (plant fiber based) has been shown to be good for our gut health as much as avoiding processed food rich in sugar, trans-fat, refined flour etc. This, in addition to maintaining an active and a positive approach to life (easier said than done, right?) should keep our microbes a happy bunch.
Finally, from a scientific standpoint, what we know is probably, a small speck on the tip of an iceberg. However, the field is now beginning to explode with the advent of sensitive genomic sequencing tools and multi-omics approaches, generating a lot of interest with regards to diagnostic as well as therapeutic approaches. The clinical significance of genetic signature of the microbiome, is only beginning to be understood by the scientific community which certainly will add great value for precision medicine.
- Ye et al., Cancer Biol. Ther., 2024, DOI: 10.1080/15384047.2024.2306676
- Zhang et al., Front. Immunol., 2024, doi: 10.3389/fimmu.2023.1338918. eCollection 2023
- Chang et al., Biomed. J. 2024, doi: 10.1016/j.bj.2024.100698
- Cui et al., Biomech Pharmacother., 2024, doi: 10.1016/j.biopha.2024.116203
- Otsuka et al., Cancer Immuno Immunother., 2024, doi: 10.1007/s00262-023-03608-y
- https://link.springer.com/article/10.1007/s12038-021-00182-2
- https://mapi.com/blogs/articles/gut-health-microbiome-ayurveda
- https://www.ddw-online.com/results-for-microbiome-based-immuno-oncology-drug-expected-h1-2024- 28074-202401/
- Author : Dr. Dhanalakshmi S- Chief Scientific Officer at TheraIndx Lifesciences Private Limited